Claim Denial Vs Rejection What S The Difference Medical ођ
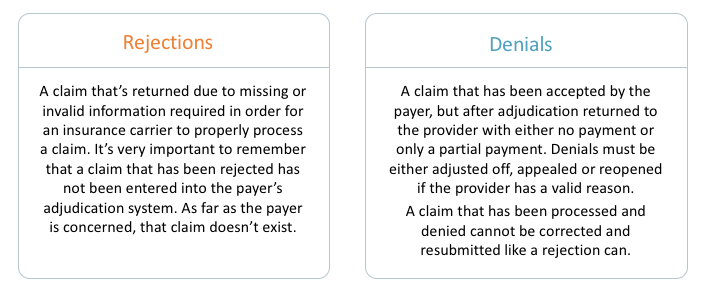
Understanding The Medical Claims Process To Get Paid Kareo Definitions of denial vs. rejection claim denial. claim denial happens after the claim has undergone processing and adjudication. once the claim is accepted by the payer, it is thoroughly reviewed to match the patient’s benefits and the payer’s medical policies. if any discrepancies are found during this review, the claim may be denied. Evaluation status: a denial means the claim was fully evaluated and payment was denied based on the policy. a rejection means the claim could not be processed as is due to problems that make evaluation impossible. completeness: denied claims are complete and finalized claims. rejected claims are considered incomplete claims.
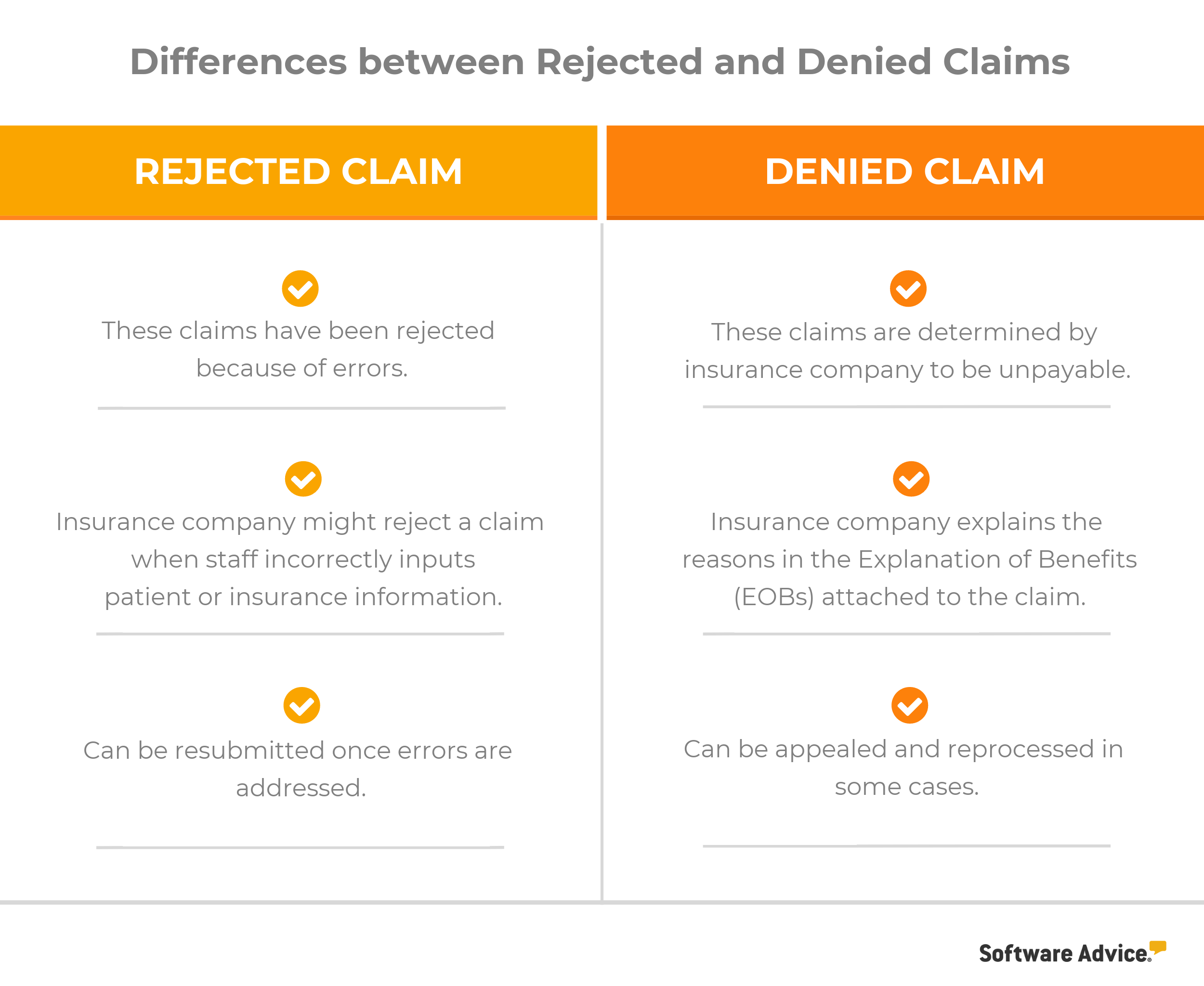
5 Ways To Avoid Common Medical Claim Errors Denials are often more complex and can be harder to resolve than rejections. common reasons for claim denials include lack of coverage for the service provided, missing prior authorization, or non compliance with the payer’s policies. for example, if a patient receives a non covered service or visits an out of network provider, the claim may. Claim rejections occur when a medical claim fails to meet specific criteria of either the payer or x12 standardization. unlike denials, claim rejections happen before the claim is processed. a claim rejection usually comes from errors in data entry, formatting issues and missing information. as a result, the claim never enters the payer’s. Insurance claim denials and rejections are one of the biggest obstacles affecting healthcare reimbursements. too often the terms “claim rejection” and “claim denial” are used interchangeably in the billing world. this misunderstanding can create very costly errors and can have a significant, negative impact on your overall revenue cycle. These terms are frequently used to discuss medical billing claims and are often used interchangeably by even the most experienced team members in the health field. however, a rejection differs vastly from a denial. additionally, the processes necessary to effectively overturn the ruling of a rejection is different from that of a denial.
Medical Claim Denials And Rejections In Medical Billing Insurance claim denials and rejections are one of the biggest obstacles affecting healthcare reimbursements. too often the terms “claim rejection” and “claim denial” are used interchangeably in the billing world. this misunderstanding can create very costly errors and can have a significant, negative impact on your overall revenue cycle. These terms are frequently used to discuss medical billing claims and are often used interchangeably by even the most experienced team members in the health field. however, a rejection differs vastly from a denial. additionally, the processes necessary to effectively overturn the ruling of a rejection is different from that of a denial. Claim rejections are most commonly caused by the information on the claim not matching the information in the payer’s system (examples: misspelt client names, incorrect provider npi numbers, incorrect client insurance identification numbers, etc.) fixing a claim rejection is usually just fixing the incorrect information in your ehr system and. We’ve seen that most denied claims fail during the processing stage. rejected claims come back to the biller before the insurance company has processed anything, usually because they contain errors. these rejected claims never make it into the insurance company’s system. in some cases, they never make it out of the medical biller’s.

Comments are closed.